|
Written by Sureshi Jayawardene October is breast cancer awareness month. During this time awareness campaigns advocate nationally for early testing and diagnosis. The American Cancer Society (ACS) has been key in these efforts and, in the past, has taken an aggressive approach to screening, recommending that women age 40 and older have mammograms and clinical exams annually. However, on October 20th 2015, the organization issued new guidelines for mammograms. They said that women should begin mammograms later and have them less frequently. According to their announcement, the ACS recommends women with an average risk of breast cancer start having mammograms at age 45 and continue annually until 54. Following this, they recommend screenings every other year so long as women remain healthy. In addition, the organization states that women who have experienced no symptoms or breast abnormalities need no longer have clinical breast exams. A clinical breast exam is when a nurse or doctor feels for lumps. The ACS also notes that mammograms are less useful for younger women and inconsistencies such as false positive results can unnecessarily lead to additional testing including biopsies.
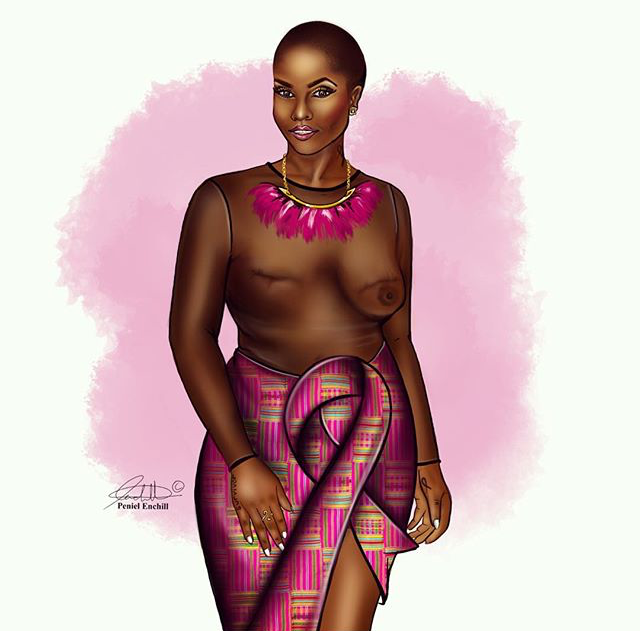
BLACK WOMEN AND BREAST CANCER These guidelines have been met with some disagreement from organizations especially concerned with minority communities. For instance, the Mayo Clinic indicates that breast cancer affects Black women at a younger age than other groups and that tumors can be significantly more aggressive. African American women are also less likely to take action early enough. Linda Goler Blount, president and CEO of Black Women’s Health Imperative highlights the role of health insurance in this situation. According to her, African American women are 45% less likely to have health insurance than White women and have a 40% greater mortality rate as a result of breast cancer. In their recent study, Keenan et al (2015) state that these racial disparities in tumor outcomes between White and Black women might be explained by more aggressive tumor biology in Black women. Each year, approximately 6,000 Black women die from breast cancer. If the mortality rate for Black women equaled that of White women, these deaths would be reduced by 2,400. The ACS should take into consideration the racial disparities of breast cancer so that early detection and other treatment mechanisms can be made available for Black women. If African American women are able to have early detection of their cancer – which is the period when they are most successfully treated and women can receive quality treatment – fewer women would die. CULTURE AND BREAST CANCER PREVENTION Health professionals and researchers need to look at cultural factors as an initial step toward addressing the failures of breast cancer prevention and control strategies (Guidry et al., 2003). While ethnic and ancestral factors may differ among women of African descent, “there remains a set of shared beliefs, values, and experiences that researchers should understand when evaluating the importance of culture in breast cancer prevention and control” (Guidry et al., 2003, p. 319). To this end, such programs need to be consistent with cultural components in the Black community. Some of these include attitudes toward kinship bonds, flexible family roles, religiosity, education, and work (Guirdy et al., 2003). Community-based interventions can be effective in connecting Black communities to health agencies. These often work to establish social networks, serve as a resource, and offer social support (Guidry et al., 2003). Some of the most noteworthy community-based initiatives include Save Our Sisters Project, the North Carolina Breast Cancer Screening Program, and the Witness Project. Not only have these programs been sensitive to the culturally specific needs of their Black women patients, but have positively influenced breast cancer screening behavior among their target population (Guidry et al., 2003). Thus, attending to the cultural and psychosocial factors in through community health services can yield positive outcomes for Black women in terms of breast cancer awareness, treatment, and support. WHAT CAN BLACK WOMEN DO NOW? Given the new ACS guidelines and the additional health related burdens faced by Black women socially and economically, learning about risks for breast cancer are crucial. For Black women under 40, seeking your physician’s advice about your particular risk factors can be beneficial as well as finding out whether a base line mammogram is necessary. For women over 40, making a mammogram an annual occurrence is important. Under the Affordable Care Act, mammograms are a covered benefit with no cost to the patient. In addition, learning about local and regional community health initiatives and other resources can also prove helpful. BREAST CANCER RESOURCES FOR BLACK WOMEN
Works Cited Guidry, J.J., Matthews-Juarez, P., and Copeland, V.A. (2003). Barriers to breast cancer control for African-American women: The interdependence of culture and psychosocial issues. Cancer 97 (1 supplemental): 318-23. Keenan, T., Moy, B., Mroz, E.A., Ross, K., Niemierko, A., Rocco, J.W., Isakoff, S., Ellisen, L.W., and Bardia, A. (2015). Comparison of the genomic landscape between primary breast cancer in African American versus White women and the association of racial differences with tumor recurrence. Journal of Clinical Oncology. DOI 10.1200/JCO.2015.62.2126
0 Comments
Leave a Reply. |
Archives
April 2022
Categories
All
|
 RSS Feed
RSS Feed